anatomy and physiology of heart pdf
The heart is a vital organ essential for maintaining life, responsible for pumping blood throughout the body. Its anatomy and physiology are complex, involving layers like the epicardium, myocardium, and endocardium. Understanding its structure, including chambers and valves, is crucial for grasping its function in circulation. This knowledge aids in diagnosing and treating heart conditions, emphasizing the importance of studying cardiac anatomy and physiology.
1.1 Overview of the Heart’s Importance in the Circulatory System
The heart is the central organ of the circulatory system, responsible for pumping blood throughout the body. It ensures oxygen and nutrients are delivered to tissues while removing waste products, maintaining cellular function and overall health.
Without the heart’s continuous operation, blood cannot circulate, leading to tissue damage and organ failure. Its role is vital for sustaining life, making it the cornerstone of the circulatory system.
1.2 Brief History of the Study of Heart Anatomy and Physiology
The study of heart anatomy and physiology dates back to ancient times, with significant contributions from William Harvey in 1628, who first described blood circulation. Modern research, such as a 2018 study on the ductus arteriosus and a 2022 review, highlights ongoing advancements in understanding cardiac structure and function, building on historical discoveries to refine current knowledge.

Gross Anatomy of the Heart
The heart is a cone-shaped organ, approximately the size of a clenched fist, centrally located in the thoracic cavity. It lies between the lungs, slightly to the left of the midline, playing a crucial role in the circulatory system by pumping blood efficiently.
2.1 Location and Position of the Heart in the Thoracic Cavity
The heart is centrally located in the thoracic cavity, nestled between the lungs, and slightly offset to the left of the midline. This positioning allows for efficient blood circulation to both the pulmonary and systemic systems. The heart’s apex points downward, while its base faces upward, ensuring optimal blood flow through its chambers and into the great vessels surrounding it.
2.2 Pericardium and Its Role in Heart Function
The pericardium is a double-layered sac enclosing the heart, providing protection and reducing friction between the heart and surrounding structures. It consists of a fibrous outer layer and a serous inner layer, which secretes pericardial fluid to lubricate heart movements. The pericardium stabilizes the heart’s position in the thoracic cavity and plays a crucial role in maintaining cardiac function by preventing excessive movement and ensuring efficient blood circulation.
Microscopic Anatomy of the Heart
The heart’s microscopic anatomy reveals three distinct layers: the epicardium, myocardium, and endocardium. These layers work together to regulate cardiac function, ensuring efficient blood circulation.
3.1 Layers of the Heart: Epicardium, Myocardium, and Endocardium
The heart comprises three layers: the epicardium, the outermost layer protecting the heart; the myocardium, the thick muscular middle layer enabling contraction; and the endocardium, the inner lining of chambers and valves. These layers collaborate to maintain cardiac structure and function, ensuring proper blood flow and overall cardiovascular health.
3.2 Cardiac Muscle Structure and Function
Cardiac muscle, found exclusively in the heart, is responsible for its rhythmic contractions. It exhibits unique features like striations, intercalated discs, and branching fibers, enabling synchronized contractions. Its function is inherently rhythmic, with contractions initiated by the sinoatrial node, ensuring consistent blood circulation without external stimulation, making it vital for maintaining life and overall cardiovascular efficiency.
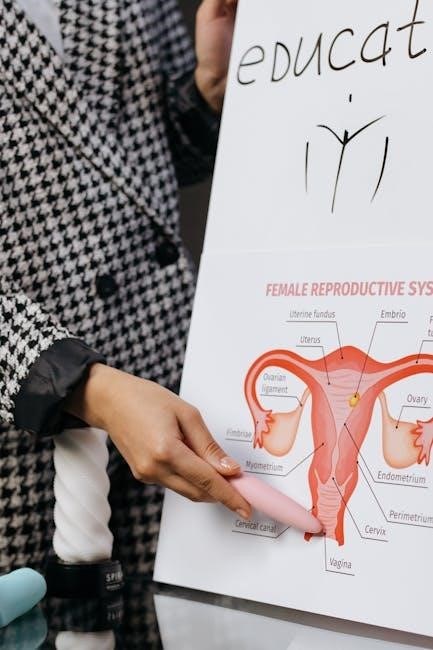
Chambers of the Heart
The heart contains four chambers: the left and right atria, and the left and right ventricles. The atria are thin-walled, while the ventricles are thicker, enabling efficient blood propulsion.
4.1 Right Atrium and Left Atrium
The right atrium (RA) and left atrium (LA) are the upper chambers of the heart. The RA receives deoxygenated blood from the body via the superior and inferior vena cava. The LA receives oxygenated blood from the lungs via the pulmonary veins. Both atria function as reservoirs and auxiliary pumps, ensuring efficient blood flow into the ventricles during diastole.
4.2 Right Ventricle and Left Ventricle
The right ventricle (RV) pumps deoxygenated blood to the lungs via the pulmonary artery, while the left ventricle (LV) pumps oxygenated blood to the body through the aorta. The LV has a thicker muscular wall compared to the RV due to the higher pressure required for systemic circulation. Both ventricles play critical roles in maintaining blood flow and overall cardiac function, with their contractions synchronized by the heart’s conduction system.
Valves of the Heart
The heart contains four valves: mitral, tricuspid, aortic, and pulmonary. These valves regulate blood flow direction, ensuring efficient circulation and preventing backflow, which is vital for heart function.
5.1 Structure and Function of the Mitral and Tricuspid Valves
The mitral and tricuspid valves are crucial for unidirectional blood flow. The mitral valve, located between the left atrium and ventricle, has two leaflets, while the tricuspid valve, situated between the right atrium and ventricle, has three. Both are supported by chordae tendineae and papillary muscles, ensuring proper closure during systole to prevent regurgitation and maintain cardiac efficiency.
5.2 Role of the Aortic and Pulmonary Valves
The aortic and pulmonary valves are critical for directing blood flow from the ventricles. The aortic valve, located at the base of the aorta, ensures blood flows from the left ventricle into the systemic circulation. The pulmonary valve, at the pulmonary artery’s base, directs blood from the right ventricle to the lungs. Both valves prevent backflow, maintaining efficient circulation and proper cardiac function.
Blood Circulation
Blood circulation involves the transport of oxygenated and deoxygenated blood throughout the body; It is divided into systemic and pulmonary circuits, ensuring efficient oxygen delivery and carbon dioxide removal.
6.1 Pulmonary Circulation
Pulmonary circulation transports deoxygenated blood from the right ventricle to the lungs via the pulmonary artery and returns oxygenated blood to the left atrium through the pulmonary veins. This process ensures efficient gas exchange in the alveoli, vital for oxygenating blood and removing carbon dioxide. The pulmonary circuit operates at lower pressure than systemic circulation, adapting to the lungs’ needs for gas diffusion and maintaining proper blood oxygen levels.
6.2 Systemic Circulation
Systemic circulation delivers oxygenated blood from the left ventricle to the body via the aorta and returns deoxygenated blood to the right atrium through the venae cavae. This circuit supplies oxygen and nutrients to tissues and organs, supporting cellular functions and overall metabolism. It operates at higher pressure than pulmonary circulation, ensuring efficient distribution of blood throughout the body and maintaining proper organ perfusion, regulated by the autonomic nervous system and hormones like epinephrine.
Conduction System of the Heart
The heart’s conduction system includes the sinoatrial node, atrioventricular node, Bundle of His, and Purkinje fibers. It generates and conducts electrical impulses, regulating heart rhythm and ensuring synchronized contractions.
7.1 Role of the Sinoatrial Node and Atrioventricular Node
The sinoatrial node, located in the right atrium, acts as the heart’s natural pacemaker, generating electrical impulses that initiate cardiac contractions. The atrioventricular node, situated near the septal wall, delays these impulses, ensuring proper atrial contraction before ventricular activation. This coordination maintains a consistent and efficient heart rhythm, essential for overall cardiovascular function and systemic blood circulation.
7.2 Function of the Bundle of His and Purkinje Fibers
The Bundle of His transmits electrical impulses from the atrioventricular node to the ventricles, ensuring coordinated contraction. Purkinje fibers, branching from the Bundle of His, spread the impulse across the ventricular muscle, enabling rapid and synchronized contraction. This system is crucial for maintaining proper heart rhythm and efficient blood circulation, ensuring the heart functions as a cohesive unit.
Physiology of Heart Function
The heart’s physiology involves generating and maintaining blood pressure through the cardiac cycle, ensuring oxygenated blood circulates efficiently. This process is vital for overall bodily function and health.
8.1 Cardiac Cycle and Heart Sounds
The cardiac cycle consists of phases: isovolumetric contraction, ventricular ejection, isovolumetric relaxation, rapid filling, and diastasis. Heart sounds, such as the first (S1) and second (S2), arise from valve closures. S1 occurs during atrioventricular valve closure, while S2 follows semilunar valve closure. These sounds are vital for assessing cardiac function and diagnosing abnormalities, providing insights into the heart’s mechanical activity during each cycle.
8.2 Regulation of Heart Rate and Blood Pressure
The heart rate and blood pressure are regulated by the autonomic nervous system, with the sympathetic system increasing heart rate and the parasympathetic system decreasing it via the vagus nerve. Hormones like adrenaline also stimulate heart rate. The sinoatrial node acts as the heart’s pacemaker, initiating contractions. These regulatory mechanisms ensure proper blood flow and maintain homeostasis, adapting to physiological demands such as exercise or stress.
Clinical Significance of Heart Anatomy and Physiology
Understanding heart anatomy and physiology is crucial for diagnosing and treating conditions like arrhythmias and heart failure, improving patient outcomes through targeted interventions.
9.1 Common Heart Conditions and Their Implications
Common heart conditions include arrhythmias, heart failure, and coronary artery disease, often linked to anatomical or physiological dysfunctions. Arrhythmias disrupt normal heart rhythms, potentially leading to serious complications. Heart failure reduces the heart’s pumping efficiency, affecting overall circulation. Coronary artery disease, involving narrowed arteries, can cause ischemia or infarction. Understanding these conditions is vital for early diagnosis and effective treatment, improving patient outcomes significantly.
9.2 Diagnostic Techniques for Heart Disorders
Common diagnostic techniques for heart disorders include electrocardiograms (ECG), echocardiograms, and cardiac MRI. ECG measures heart rhythm, detecting arrhythmias. Echocardiograms use ultrasound to visualize heart structures, identifying issues like valve problems. Cardiac MRI provides detailed images of heart tissue, aiding in diagnosing conditions like cardiomyopathy. These tools are essential for early detection and accurate diagnosis, guiding effective treatment plans for various heart conditions.
The heart is a vital organ central to the circulatory system, pumping blood to sustain life. Understanding its anatomy and physiology is crucial for medical advancements and treatments.
10.1 Summary of Key Concepts
The heart, a muscular organ, pumps blood through chambers and valves, enabling pulmonary and systemic circulation. Its structure includes layers like the epicardium, myocardium, and endocardium. The conduction system regulates heartbeats, while the autonomic nervous system controls heart rate and blood pressure. Understanding these elements is vital for diagnosing and treating heart conditions, emphasizing the importance of cardiac anatomy and physiology in maintaining overall health and preventing diseases.
10.2 Importance of Understanding Heart Anatomy and Physiology
Understanding heart anatomy and physiology is crucial for diagnosing and treating cardiovascular diseases. It aids in identifying structural abnormalities, such as faulty valves or chambers, and functional issues like arrhythmias. This knowledge also helps in developing preventive strategies, improving surgical techniques, and enhancing overall patient care. Studying the heart’s structure and function is essential for both medical professionals and general health awareness, promoting better cardiovascular health management and disease prevention.